Mightier Together: The Journal
Navigating chronic illness & medical devices, together.
learn by device or treatment type
Your first PICC line (Peripherally Inserted Central Catheter), will likely come with a bunch of questions. Don’t worry; we’ve got you covered.
Are you just getting a port or transitioning from PICC to Port? Here’s all the info you’ll need, including personal tips from co-founder Emily Levy.
For many people with GI challenges, eating and drinking may not be the best way to get nutrition. Click here to learn more about Feeding Tubes.
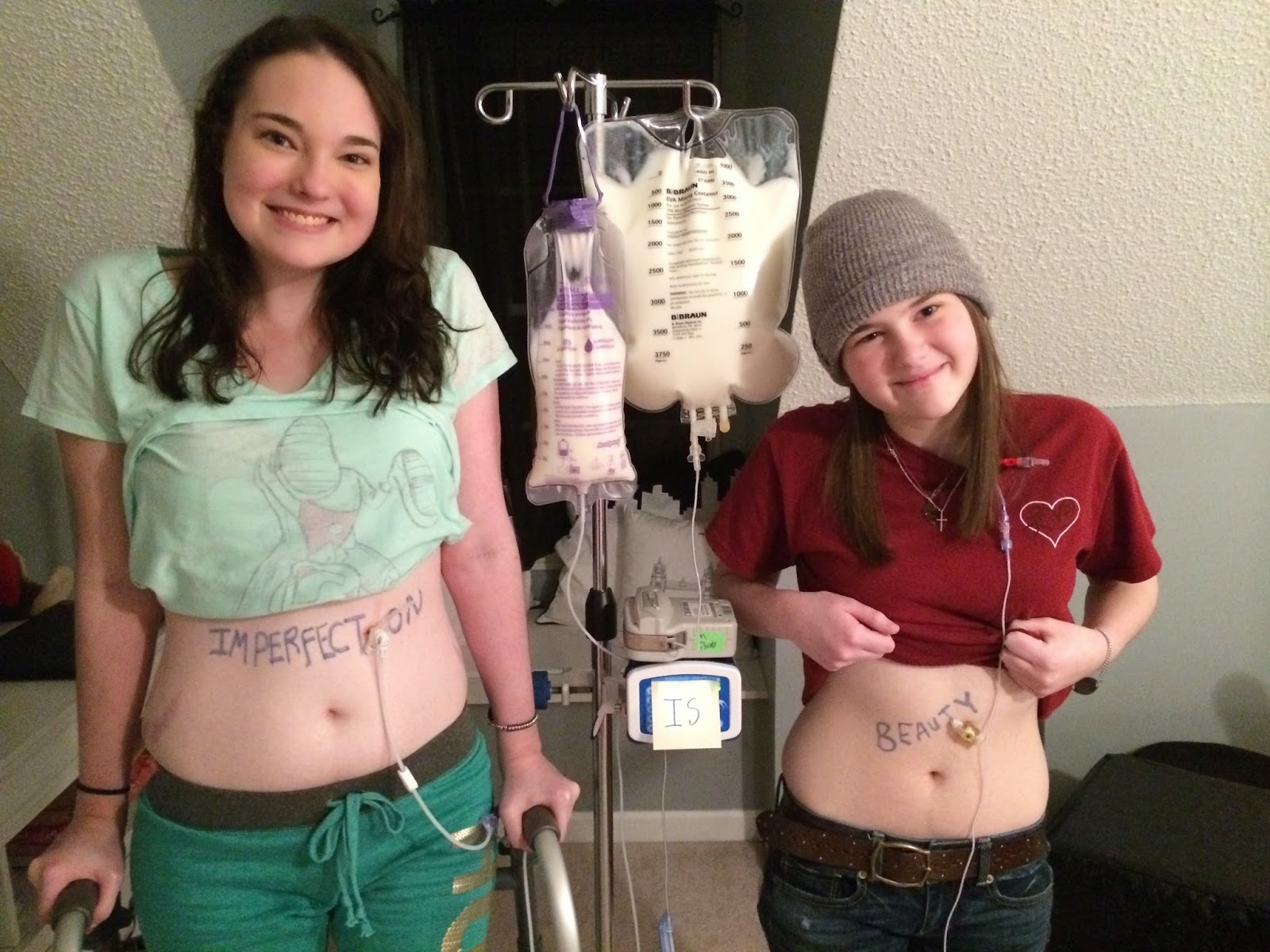
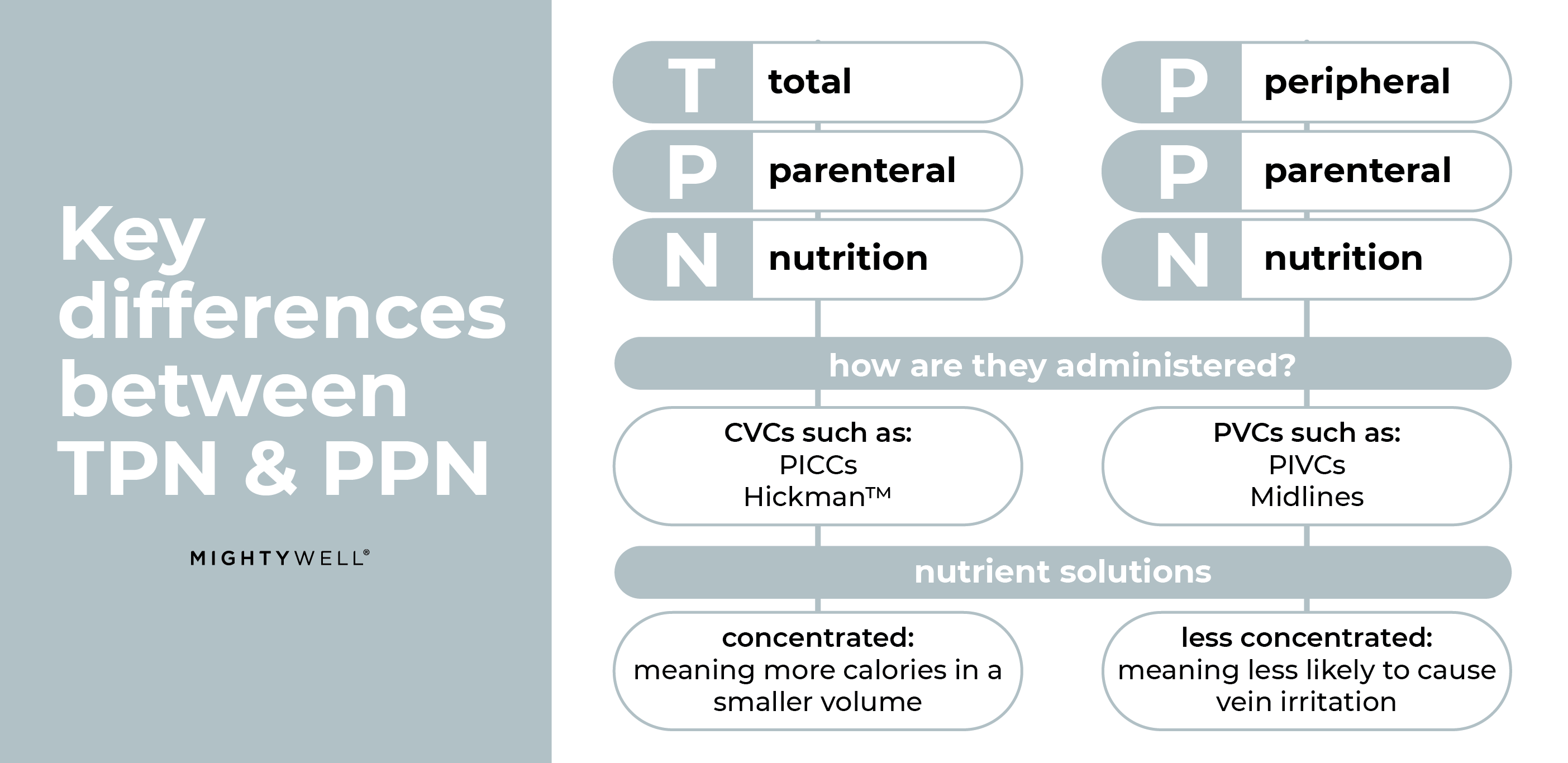
Total Parenteral Nutrition (TPN) is when nutrients are given directly into the bloodstream through a long-term intravenous catheter like a PICC. Click here to learn more about TPN.
learn by condition or diagnosis
Looking for general advice and tips on chronic illness as a whole? From patient stories to general tips, start here.
Just diagnosed with cancer and wondering what comes next, or looking to support a loved one? Check out our Cancer hub for advice and personal experiences from Friends in the Fight.
If you’ve just been diagnosed with diabetes, the good news is that plenty of research is available. Here are some tips from chatting with our diabetic Friends in the Fight.
Where Mighty Well started: get expert tips from co-founder Emily and her journey living with Lyme.
Are you looking for advice and patient stories on Multiple Sclerosis? Look no further, catch up with a few of our Ambassadors on their experiences here.